Traditional treatments for repairing a damaged or torn spinal disc leave patients with a host of side effects, and don’t consistently provide relief. The Discseel® Procedure is a revolutionary procedure using an FDA approved biologic to repair your damaged spinal disc.
It is a minimally invasive procedure that injects a biologic into intervertebral discs. This is able to repair and seal damaged spinal discs, where spine surgery, including spinal fusions, can’t.
Often people suffering from Degenerative Disc Disease are plagued with back pain from one or more torn discs, which inflame spinal nerves causing back pain and leg pain. When a disc leaks, over time it can lose hydration and become degenerated.
Your intervertebral discs are oval structures that work as cushions between your spine bones (vertebrae). These discs are made of two regions: the inner jelly-like region (Nucleaus Pulposus) and the outer harder rim (Annulus Fibrosus).
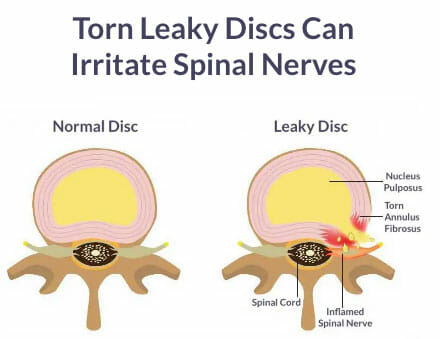

Due to age, disease or trauma, the outer rim of intervertebral discs undergoes wear and tear. The outer rim, (Annulus Fibrosus) can tear leading to leaking of the soft center out into the intervertebral canal. This frequently leads to problems like nerve irritation and back pain. Sometimes the tears are microscopic while other times they can be obvious.
The Discseel® Procedure aims at healing these tears. When injected into the targeted discs, the biologic works in two main ways. The immediate effect of the biologic includes filling up the tears in the discs. The long-term benefit is that it adds to the strength and stability of the intervertebral discs.
• Sciatica
• Degenerative disc disease (disc degeneration)
• Disc protrusion, disc herniation, slipped disc
• Disc bulge, disc prolapse
• Chronic low back pain
• Pain after Spinal Fusion
surgery
• Pain after failed back surgery
(Failed Back Surgery Syndrome).
• Disc tears, annular tear


1. Consultation. We begin by a phone consultation followed by a consultation by our Medical Director, Janet D Pearl, MD MSc. We ask you to send us your CT or MRI scan ahead of time so we can do a preliminary evaluation. Then, if we think you are a suitable candidate, we’ll have you come in for a in-person consultation to meet with our Medical Director, Janet D Pearl MD MSc who will perform the Discseel® Procedure. We want to answer all your questions prior to the procedure.
2. Annulogram. The annulogram is a pain free fluoroscopic X-Ray examination of your discs. We inject a small amount of X-Ray contrast into the outer rim of your intervertebral discs. This determines if your discs are leaking. We can identify very small subtle disc tears (even before they cause herniation or degeneration.) Anything missed by an MRI or CT will show up in the annulogram.
3. Discseel® Procedure. Immediately after the annulogram, we inject the biologic into each damaged disc, which seals the leaks. The biologic used is an FDA approved biologic that is made from human blood. The entire procedure is done live under x-ray guidance.
4. Recovery. After the procedure most patients are up and walking within 24 hours. Immediately after the procedure, your damaged discs will start healing, which is a continuous process over the next 12 months. Most patients experience relief at 3-6 months post procedure because our discs heal slowly.
A 2020 study of 320 patients that is pending publication reports that: “Statistically significant improvement was realized in every outcome tool comparing baseline to; 3-months, 6-months, and 1-year post-treatment. No subject was lost to follow-up or withdrawn, and no subject experienced an adverse event. The results of the longitudinal analysis demonstrated statistically “significant improvement in all outcomes measured.” See below for details.
2020 ABSTRACT PENDING PUBLICATION:
EVALUATING THE SAFETY AND EFFICACY OF FIBRIN TO TREAT MULTI-LEVEL CHRONIC DISCOGENIC LOW BACK PAIN
BACKGROUND:
Chronic low back pain is the most common cause of disability worldwide, and to date, no surgical or non-surgical treatment has been shown to reliably provide relief in treating chronic low back pain. Lumbar discs are the most common cause of chronic low back pain, and so this investigation evaluates the safety and efficacy of using non-autologous fibrin, introduced intra-annularly, to treat annular defects causing chronic low back pain. Annulogram is a dynamic test, identifying annular defects and contrast flow patterns within the 22-25 annular layers. Annulograms possess greater sensitivity than does MRI in identifying annular defects, and this dynamic test is somewhat analogous to coronary arteriograms, another dynamic test initially fraught with skepticism before it’s widespread acceptance which changed the paradigm evaluating CAD. Favorable results of ongoing investigations suggest that annulograms will be a mainstay in treating spine pathology. Previous published in vivo investigations demonstrate fibrin’s ability to mechanically repair annular defects and stimulate new disc growth, returning all disc biochemical and mechanical properties to normal. This investigation evaluates the amalgam of refinements meant to improve clinical outcome.
PURPOSE:
To evaluate the safety and efficacy of intra-annular fibrin to treat chronic low back pain. Compared to many prior investigations, this investigation evaluates the amalgam of diagnostic and therapeutic refinements meant to improve patient outcomes, including: (1) Diagnostic Annulograms used to identify annular defects; (2) Targeting fibrin to those Annulus Fibrosus defects; and (3) Treating each disc in the region of symptoms. of Subjects were treated by the Principle Investigator, and subjects prospectively reported their outcome measures in the Regenerative Orthobiologics Registry (ROR). Outcome tools measured; pain, physical function, mental health, quality of life, satisfaction, and adverse events, to evaluate the safety and efficacy of intra-annular non-autologous fibrin in treating patients with moderate to severe chronic low back pain.
STUDY DESIGN:
Prospectively reported outcome measures analyzed retrospectively in the ROR.
PATIENT SAMPLE:
Subjects suffering from low back pain, with or without leg pain, for greater than six months duration, who failed prior treatments, including; intra-discal stem cell or precursor cell injections (BMAC), as well as intra-discal PRP, zygapophyseal joint (facet joint) “stem cell or PRP injections,” physical therapy, fluoroscopically-guided transforaminal or interlaminar epidural injections of corticosteroid, radiofrequency neurotomy, or medial branch blocks to rule out posterior element pain. Several subjects failed to experience relief following surgical discectomy and fusion.
OUTCOME MEASURES:
VAS low back; VAS leg; Numeric Rating Scale (NRS); Bodily Pain; Estimated Utility Score; PROMIS Global Mental Health; Global Physical Health; NASS Patient Satisfaction Index Score; Oswestry Disability Index (ODI); and EuroQuol.
METHODS:
320 Subjects with chronic low back pain (LBP) who failed to experience relief following prior spine treatments underwent a screening lumbar MRI and x-ray. Patients without severe vertebral canal stenosis or spinal instability, as determined by lumbar MRI and lateral X-ray, respectively, were enrolled in this investigation. All subjects reported their pre-treatment outcome measures in the ROR, and then underwent diagnostic anulograms, with subsequent intra-annular injection of non-autologous fibrin to treat annular defects of all morphologically abnormal intervertebral discs in the region of symptomology. Subjects reported their pre- and post-treatment outcome measures beginning in 2017 to present, assessing; pain, physical function, mental health, quality of life, and patient satisfaction.
RESULTS:
Statistically significant improvement was realized in every outcome tool comparing baseline to; 3-months, 6-months, and 1-year post-treatment. No subject was lost to follow-up or withdrawn, and no subject experienced an adverse event. The results of the longitudinal analysis demonstrated statistically significant improvement in all outcomes measured.
CONCLUSIONS:
Patients with chronic low back pain underwent diagnostic annulograms to identify disc annular defects, and those defects were repaired using intra-annular injection of non-autologous fibrin. Subjects prospectively reported statistically significant improvement of all outcomes at; 3, 6, and 12 months post-treatment, with no adverse events.
A 2020 study of 320 patients that is pending publication reports that: “Statistically significant improvement was realized in every outcome tool comparing baseline to; 3-months, 6-months, and 1-year post-treatment. No subject was lost to follow-up or withdrawn, and no subject experienced an adverse event. The results of the longitudinal analysis demonstrated statistically significant improvement in “all outcomes measured.”
Any person with long lasting low back pain is a potential candidate. A person with low back pain who’s had surgery or a person with low back pain who prefers to avoid surgery is also a potential candidate, because the cushion in the back known as the disc is the most common cause of low back pain. Contact us to find out if you are a candidate.
No. We use conscious sedation during the procedure, so it is not painful or uncomfortable for our patients. Conscious sedation is a combination of medicines to help you relax (a sedative) and to block pain (an anesthetic) during a medical procedure. Under conscious sedation, you may fall asleep, but you will wake up easily to respond to people in the room. You may be able to respond to verbal instructions. After conscious sedation, you may feel drowsy and not remember much about your procedure, but you will recover quickly and we encourage you to begin walking the next day.
This is an outpatient procedure done in a morning or afternoon. You will likely need a few days to rest, however, we want you up and walking around the day following your procedure. After the first few days, when you are feeling up to it, we want you to begin a daily regimen of walking, gradually building up your walking distance every few weeks. Most people need prescription pain medication for the first few weeks.
Most people see a change within 3 – 6 months after the Discseel® procedure, and some are sooner than that. Most people are back at work the week after their procedure. It is normal to experience increased symptoms after your procedure and then go through a period of time where the pain waxes and wanes for several months.
The main thing to remember following your procedure is to avoid two movements: flexion (forward bending) and rotation (twisting). Flexion is a compressive force and rotation is a shear force, both of which can damage and tear discs. Many people ask, “How long do I have to avoid those movements?” We encourage all patients to avoid these movements as a lifestyle because we know these are the two forces that can damage and tear discs. We recommend working with a physical therapist for a short period of time following the procedure to learn new body mechanics in order to avoid movements that cause wear and tear on the discs.
It can take 3 – 12 months for the disc to be restored and for you to have noticeably decreased pain and improved function. Beginning the day of your procedure, your discs will begin the healing process. Most patients experience increased symptoms following the procedure for several weeks and do not notice significant change from their usual pain for 3-6 months. Occasionally some notice a quick difference, but that is the exception, not the norm.
We will work with your prescriptions and provide pain medications immediately following your procedure. If you are an out of state patient, because of pharmacy regulations, we ask that you follow up with a pain management doctor in your hometown before your prescription runs out if you need to continue medications to manage your pain.
A 2020 study of 320 patients that is pending publication reports that: “Statistically significant improvement was realized in every outcome tool comparing baseline to; 3-months, 6-months, and 1-year post-treatment. No subject was lost to follow-up or withdrawn, and no subject experienced an adverse event. The results of the longitudinal analysis demonstrated statistically significant improvement in “all outcomes measured.”
Early disc treatments were initially performed over 14 years ago to establish patient safety and demonstrate Fibrin’s ability to allow patients to avoid spine surgery. We have substantially refined the process since then:
Intradiscal injection of fibrin sealant for the treatment of symptomatic lumbar internal disc disruption: results of a prospective multicenter pilot study with 24-month follow-up. Yin W, Pauza K, Olan WJ, Doerzbacher JF, Thorne KJ.; Pain Med. 2014 Jan;15(1):16-31. doi: 10.1111/pme.12249. Epub 2013 Oct 23. Link to article
Discseel® Regenerative Spine Procedure Website. Link to website
Treatment of annular disc tears and “leaky disc syndrome” with fibrin sealant. Pauza K MD, Wright C BS, Fairbourn A Best, Mark.; Techniques in Regional Anesthesia and Pain Management Vol 19, Iss 1–2, Jan–Apr 2015: 45-49. Link to article
Intradiscal Biologic Treatments: Intra-annular Fibrin Disc Sealant. Kevin Pauza MD; Advanced Procedures for Pain Management: A Step by Step Atlas; Ed: Diwan S , Deer TR, 1st Ed, 2018 Edition pp 525-536.
Fibrin Injection Stimulates Early Disc Healing in the Porcine Model. Buser Z, Kuelling F, Jane L, Liebenberg E, Tang J, Thorne K, Coughlin D, Lotz J; The Spine Journal 9(10) · October 2009 Link to Article
Spinal Fusion for Chronic Low Back Pain: A ‘Magic Bullet’ or Wishful Thinking? Dhillon KS.; Malays Orthop J. 2016 Mar; 10(1): 61–68.
Although Stem Cell Therapy is considered by some people to be experimental, various research studies show that regenerative stem cell therapy and platelet rich plasma injections can provide excellent relief from joint and musculoskeletal pain and ongoing inflammation.
IMPORTANT! This information is for educational purposes only and is NOT intended to replace the care or advice given by your physician. Boston Applied Biologics is not offering regenerative cell therapy or other regenerative therapies as a cure for any condition, disease, or injury. No statements or implied treatments on this website have been evaluated or approved by the FDA. This website contains no medical advice. All statements and opinions provided by this website are provided for educational and informational purposes only and we do not diagnose or treat via this website or via telephone. We do not claim that any applications, or potential applications, using autologous regenerative cells and other regenerative cells are approved by the FDA, or are even effective. We do not claim that these treatments work for any listed nor unlisted condition, intended or implied. Always seek the advice of your physician or other qualified health provider before starting any new treatment or with any questions you may have regarding a medical condition. For more information see our Medical Disclaimer.
Copyright © 2025 Boston Applied Biologics, LLC. All Rights Reserved.

How Orthobiologic Therapy can relieve your joint, muscle and tendon pain without surgery so that you can get back to enjoying your life*
We are committed to your privacy. Boston Applied Biologics uses the information you provide us to contact you about relevant content, products, and services. By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy. You may unsubscribe from these communications at any time.